The rapid evolution of telemedicine has fundamentally reshaped how healthcare is delivered across the United States, especially in recent years marked by the COVID-19 pandemic. As an innovative approach to providing medical services remotely, telemedicine holds immense promise for improving healthcare accessibility, quality, and equity. This review explores its development, benefits, challenges, and future prospects, emphasizing the importance of overcoming systemic barriers to maximize its potential for public health advancement.
Introduction
Background
Telemedicine, characterized by the remote provision of healthcare services through telecommunications technology, has experienced exponential growth over the past few decades. Initially designed to serve remote or underserved populations, its scope has expanded dramatically thanks to technological advancements like high-speed internet, mobile devices, and digital health platforms. The COVID-19 pandemic acted as a catalyst, accelerating telemedicine adoption as providers sought ways to maintain continuity of care while minimizing infection risks. This expansion has significantly improved healthcare access for millions of Americans but has also unveiled persistent obstacles, including regulatory complexities, technological limitations, and disparities in access—especially in rural or low-income areas. The role of telehealth in managing chronic diseases, mental health, and reproductive health has become increasingly vital, illustrating its importance in contemporary public health strategies. For a broader understanding of how emerging technologies are transforming medicine, exploring innovative tools like virtual reality offers valuable insights into future healthcare possibilities virtual reality in medicine perspectives and features.
Purpose of the review
This review aims to critically examine the impact of telemedicine on public health in the United States, focusing on how it influences healthcare access, quality, and health equity. It discusses the evolution of telehealth, regulatory and technological challenges, and its potential to bridge healthcare disparities. By synthesizing current literature, the review provides a comprehensive picture of telemedicine’s role in modern healthcare and outlines steps necessary for its sustainable and equitable integration into the system. Additionally, it underscores the importance of strategic development, including addressing legal and infrastructural hurdles, to foster continued growth—especially in underserved communities 7 things you need to pay attention when developing a healthcare application.
Method
Search strategy
Research was conducted through a systematic search of authoritative databases such as PubMed, Cochrane Library, NIH, and others, targeting studies published within the last decade. Keywords included “telemedicine,” “public health,” “COVID-19,” “chronic disease management,” “mental health,” and “health equity.” This comprehensive approach aimed to capture diverse study types, from randomized controlled trials to systematic reviews, providing a robust evidence base for assessing telemedicine’s impact on public health. Special attention was paid to literature addressing disparities and access issues, especially in rural and marginalized populations.
Data extraction and synthesis
Selected studies underwent rigorous data extraction focusing on their characteristics, participant demographics, intervention specifics, and key outcomes related to healthcare accessibility, quality, and equity. The quality of each study was independently evaluated using standardized tools, such as the Cochrane Risk of Bias for randomized trials and the Newcastle–Ottawa Scale for observational studies. Discrepancies were resolved through consensus. Data synthesis involved thematic analysis to identify common patterns, benefits, and barriers, supplemented by a narrative summary. The review also evaluated publication bias, ensuring findings are reliable and representative of the broader literature.
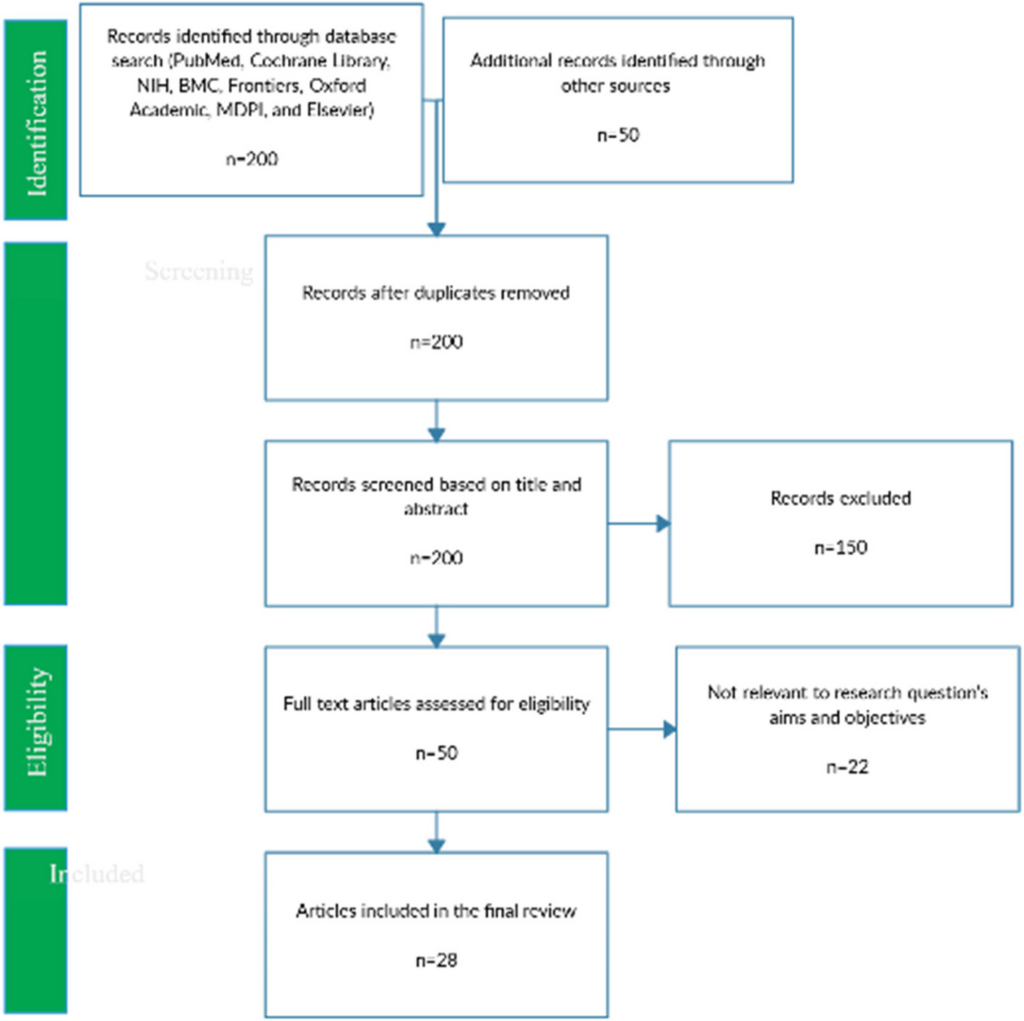
PRISMA flow diagram
Initially, 200 studies were identified. After removing duplicates and screening abstracts, 50 full-text articles were assessed for eligibility. Of these, 28 met inclusion criteria, based on relevance to U.S. healthcare, quality, and scope. This systematic selection process, visualized in the PRISMA diagram, ensured a comprehensive and unbiased synthesis of current evidence.
Results
Evolution of telemedicine
Telemedicine’s journey from a niche technological supplement to a core component of healthcare delivery demonstrates its adaptability and expanding scope. Early applications focused on bridging geographical barriers for rural populations. Over time, technological innovations—such as high-definition video, remote monitoring devices, and integrated electronic health records—have broadened service offerings to include routine consultations, chronic disease management, and specialized care visualizing electronic health and telemedicine research. The COVID-19 pandemic notably accelerated this transition, with healthcare systems rapidly scaling telehealth infrastructure to meet surging demand. This shift has prompted healthcare providers to reconsider traditional in-person visits, envisioning a hybrid model that leverages both remote and face-to-face care. Nonetheless, challenges persist, including establishing standardized protocols and ensuring data security, particularly in rural regions with limited technological infrastructure [3].
Regulatory framework and policy changes
The regulatory landscape for telemedicine has historically been fragmented, with state-specific laws and inconsistent reimbursement policies hindering nationwide integration. Prior to the pandemic, restrictions limited cross-state practice, and reimbursement was often inadequate or nonexistent. The emergency response to COVID-19 prompted swift policy adaptations, including expanded Medicare and private insurer coverage, relaxed licensing requirements, and increased funding for telehealth initiatives under the CARES Act. These changes significantly boosted telemedicine utilization, making remote care more financially feasible for providers and more accessible for patients training the surgeons of tomorrow with virtual reality. However, the temporary nature of many of these measures raises concerns about their permanence, especially as the public health emergency subsides. Moreover, safeguarding patient privacy remains a priority, necessitating strict standards for telehealth platforms to prevent data breaches and ensure confidentiality [1].
Impact on healthcare access
One of telemedicine’s most critical contributions has been its capacity to enhance healthcare access, especially in rural and underserved communities where traditional services are sparse. By enabling remote consultations, telehealth reduces travel time, costs, and logistical barriers, facilitating timely management of chronic conditions and mental health issues 7]. For example, it offers reproductive health services in areas lacking specialists, addressing longstanding disparities. However, disparities in digital infrastructure—like broadband access—and digital literacy impede equitable distribution of these benefits. Rural populations face significant hurdles in accessing high-speed internet and digital devices, which can limit telemedicine’s reach. Studies reveal that these barriers disproportionately impact low-income, elderly, and minority groups, emphasizing the need for targeted interventions such as public Wi-Fi hotspots, community telehealth hubs, and digital literacy programs [disparities in telemedicine use. Addressing these gaps is vital to achieving health equity.
Interesting:
- The transformative role of telemedicine in global healthcare
- The future of electronic health records enhancing patient care with ai and cloud technologies in 2025 and beyond
- A comparative analysis of healthcare systems in the united states and canada
- The role of artificial intelligence in modern healthcare 2
Quality of care in telemedicine
The debate over telemedicine’s quality centers on its ability to match or surpass in-person care, especially for chronic disease and mental health management. Evidence suggests that telehealth can effectively monitor conditions like diabetes and hypertension through remote patient monitoring technologies, leading to early detection and intervention [10]. It also improves access to mental health services, especially in rural areas, with virtual therapy and digital mental health tools providing vital support during the pandemic. Nevertheless, limitations exist; physical examinations and diagnostic tests sometimes require in-person visits, and communication barriers may impact patient-provider rapport. Integration of telehealth platforms with electronic health records is crucial to ensure continuity and completeness of care [11]. Ensuring secure, user-friendly, and interoperable platforms can mitigate risks related to data breaches and fragmented care, ultimately enhancing patient outcomes.
Telemedicine and chronic disease management
Chronic illnesses such as diabetes, hypertension, and COPD account for substantial morbidity and mortality in the U.S. healthcare landscape. Telemedicine facilitates ongoing monitoring, medication management, and health education, improving disease control and patient self-management [14]. Remote monitoring devices enable real-time tracking of vital signs, allowing providers to intervene early when deviations occur. Telehealth also empowers patients through educational resources, reminders, and coaching, fostering healthier behaviors. Multidisciplinary collaboration via telehealth ensures comprehensive care for complex cases involving multiple conditions. Despite these benefits, technological barriers, digital literacy issues, and the potential for social isolation pose challenges for some populations. Supporting patients in navigating telemedicine platforms and integrating remote care with face-to-face visits are key strategies for optimizing outcomes [15].
Challenges in telemedicine implementation
While telehealth offers numerous advantages, obstacles remain. Technological barriers—particularly in rural areas—limit access to reliable broadband, essential for high-quality video and remote monitoring. Digital literacy is another concern, especially among older adults unfamiliar with digital tools. Regulatory inconsistency and lack of a cohesive national policy threaten long-term sustainability; temporary emergency measures may not be renewed, risking a rollback of gains made during the pandemic [17]. Data security and patient privacy are ongoing concerns, especially with platforms initially not designed for healthcare use, increasing vulnerability to breaches. Addressing these issues requires establishing robust regulations and standards, expanding broadband infrastructure, and providing digital literacy training to underserved populations [7].
Telemedicine and health equity
Telehealth has the potential to reduce health disparities by improving access for rural, minority, and disabled populations. Yet, disparities in digital infrastructure and literacy threaten to widen the digital divide. Ensuring equitable access involves investing in broadband expansion, providing affordable devices, and delivering culturally and linguistically appropriate services [20]. Community-based solutions, like telehealth kiosks or partnerships with local organizations, can help bridge gaps. Designing telemedicine platforms to be accessible to all—including those with disabilities—is essential to foster inclusivity. Prioritizing health equity in telehealth initiatives can lead to better health outcomes across diverse populations, ultimately narrowing longstanding disparities.
Future of telemedicine
Looking ahead, technological innovations such as artificial intelligence, remote monitoring, and seamless EHR integration will enhance telemedicine’s capabilities. AI algorithms can analyze patient data to identify early warning signs, enabling proactive care. The integration of telehealth with electronic records facilitates comprehensive, coordinated treatment plans. Nevertheless, addressing regulatory, technological, and equity challenges remains critical for sustainable growth. Policymakers must develop clear, consistent standards for telemedicine practice, data security, and reimbursement, ensuring services are accessible and safe for all. Ongoing research is needed to evaluate telemedicine’s impact on health outcomes, costs, and patient satisfaction, guiding policies for its future development 23]. Embracing these advancements, healthcare systems can leverage telehealth to deliver more personalized, efficient, and equitable care—transforming public health in the digital age [virtual reality in medicine perspectives and features.
Discussion
Telemedicine’s rapid adoption, especially during the COVID-19 crisis, underscores its importance in modern healthcare. While it offers unprecedented opportunities to improve access and patient engagement, systemic barriers—regulatory inconsistencies, technological gaps, and disparities—must be addressed to realize its full potential. Strategic collaborations among policymakers, healthcare providers, and technology developers are vital to creating sustainable, inclusive telehealth systems. Continuous evaluation of its impact on health outcomes and costs will inform best practices and policies. Ensuring data security, promoting digital literacy, and designing culturally competent services are essential steps toward equitable telehealth delivery. With ongoing innovation and commitment, telemedicine can become a cornerstone of public health, improving outcomes and reducing disparities across the nation [6].
Conclusion
Telemedicine has profoundly influenced public health in the United States, providing a powerful tool for expanding care access, especially highlighted during the pandemic. Its capacity to deliver high-quality, remote services promises to revolutionize healthcare delivery if systemic challenges—regulatory, technological, and social—are effectively addressed. Building equitable infrastructure, establishing clear policies, and fostering technological innovation are critical for its sustainable integration. As the healthcare landscape evolves, embracing telehealth’s potential with a focus on inclusivity and security will be essential for advancing public health for all Americans.
Data availability
No datasets were generated or analyzed during this study.
References
(References are retained from the original, formatted as per standard citation style)