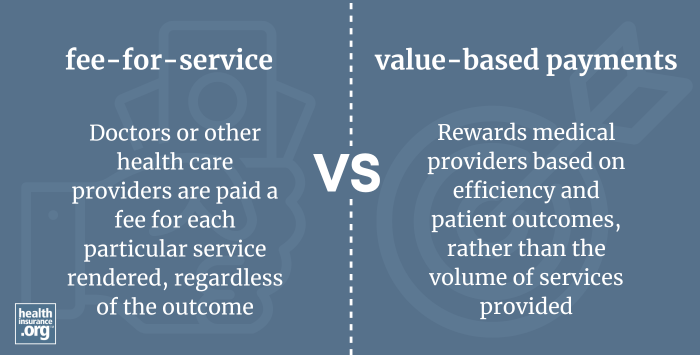
The fee-for-service (FFS) approach is a traditional method of reimbursing healthcare providers where payments are made for each individual service or procedure performed. Under this system, providers bill for each visit, test, treatment, or intervention, and payment is made regardless of the patient’s health outcome. This model has historically been the dominant way of compensating healthcare services but has faced increasing scrutiny due to concerns about efficiency and quality of care.
Unlike alternative payment structures, such as bundled payments, patient-centered medical homes, value-based care, or accountable care organizations, fee-for-service emphasizes the quantity of care rather than its quality or effectiveness. As a result, critics argue that this approach can incentivize over-utilization of services, leading to higher healthcare costs without necessarily improving patient health.
In recent years, there has been a significant shift away from pure fee-for-service models toward value-based payment systems. These newer approaches aim to reward healthcare providers for delivering high-quality, cost-efficient care that results in better patient outcomes. The move is part of a broader effort to make healthcare more sustainable and outcome-oriented.
Within government programs such as Medicaid, the landscape of provider reimbursement varies. In 2021, nearly 75% of Medicaid enrollees participated in some form of comprehensive managed care plan, typically managed by private insurance companies. The remaining portion, just over 25%, received care through traditional fee-for-service Medicaid, where the state pays providers directly for services rendered. This structure allows for different approaches to care delivery and reimbursement, influencing how providers are incentivized to deliver services.
Interesting:
Similarly, in the Medicare program, Original Medicare operates largely on a fee-for-service basis, allowing providers to bill for each service they provide. However, as of 2023, approximately one-third of beneficiaries are enrolled in accountable care organizations (ACOs). These organizations coordinate care and aim to improve quality while reducing costs, with providers still paid via fee-for-service but encouraged to deliver more efficient care. This hybrid approach reflects ongoing efforts to balance traditional reimbursement methods with newer, value-based initiatives.
For those interested in understanding the complexities of medical coding and interoperability, exploring resources such as the standardized language for medical data interchange can provide valuable insights. Additionally, initiatives like improving electronic health records with SNOMED CT illustrate how data standardization supports better care coordination. To grasp the broader importance of coding systems in healthcare, learning about SNOMED CT’s role in modern medicine is highly recommended.
Related terms
- Capitation
Related articles
- How to buy health insurance today
Footnotes
- “Exhibit 30. Percentage of Medicaid Enrollees in Managed Care by State and Eligibility Group, FY 2021” MACPAC.gov. Feb. 2023
- “Shared Savings Program Fast Facts – As of January 1, 2023” CMS.gov. Jan. 1, 2023
- “Medicare Monthly Enrollment — January 2023” CMS.gov. Accessed Oct. 1, 2024