Augmented and virtual reality (AR/VR), collectively known as extended reality (XR), are rapidly emerging as groundbreaking tools within the healthcare industry. While initially popularized through gaming and entertainment, these immersive technologies are now demonstrating vast potential in improving patient outcomes, medical training, diagnostics, and even mental health treatments. The convergence of advancing tech capabilities, increased investment, and a pressing need to address longstanding healthcare challenges has positioned AR/VR as a critical component of future medical innovation. As policymakers and industry leaders work to navigate regulatory pathways and funding opportunities, the strategic deployment of XR can significantly enhance healthcare delivery for diverse populations, especially in underserved and remote communities.
The Strategic Value of AR/VR in Healthcare
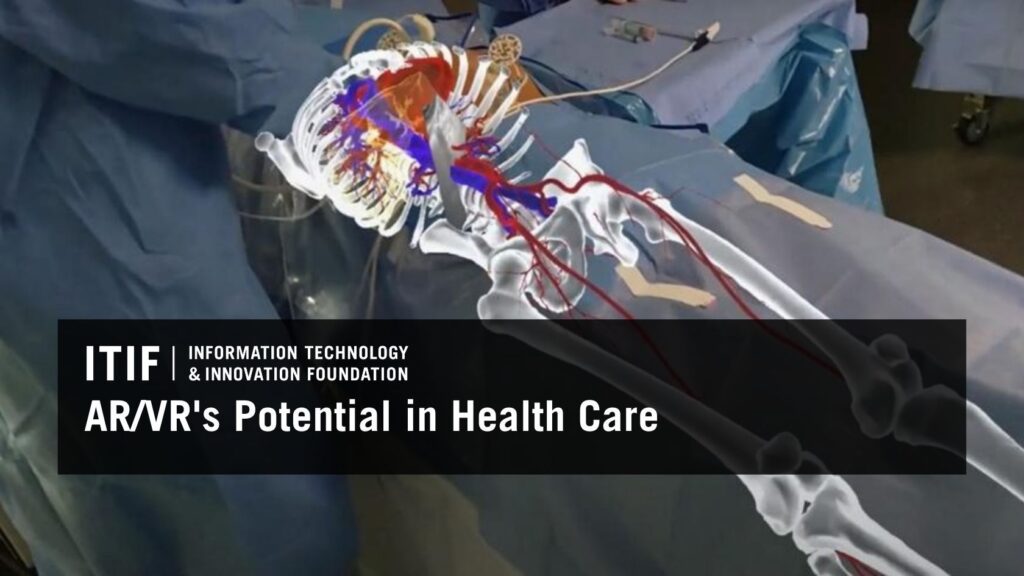
The healthcare sector has been exploring immersive tech since the early 1990s, beginning with surgical training simulators, but recent advancements have accelerated its adoption. Industry projections indicate that the AR/VR healthcare market, which was valued at around $4 billion in 2024, is expected to expand over tenfold by 2032, reaching more than $46 billion. This growth is driven by healthcare professionals’ recognition of XR’s capacity to improve precision, safety, and personalization in care delivery. For example, interactive 3D models enable clinicians to visualize complex anatomies more effectively than traditional 2D images, facilitating earlier diagnoses and more targeted treatments. Moreover, the integration of AR/VR with artificial intelligence (AI) enhances diagnostic accuracy and supports the development of digital twins—virtual replicas of patients—allowing for highly customized treatment planning and real-time monitoring.
In medical education, immersive simulations provide risk-free environments for students and practitioners to practice procedures, learn anatomy, and develop empathy across diverse patient scenarios. These tools not only improve knowledge retention—surpassing traditional methods with up to 90% recall rates—but also expand access to high-quality training regardless of geographic or resource limitations. Additionally, wearable AR/VR devices transform patient engagement by enabling at-home interventions, continuous health monitoring, and virtual consultations, thereby reducing care deserts and improving health equity. For further insights into how digital tools are revolutionizing healthcare, see the role of apps in healthcare, which highlights the importance of digital health platforms.
Who Is Benefiting from XR Technologies?
Healthcare Providers and Practitioners
AR/VR empowers clinicians to deliver more accurate, personalized, and efficient care. Surgeons utilize AR overlays to guide minimally invasive procedures with higher precision, often achieving screw placement accuracy exceeding 98%. Remote consultations are enhanced through immersive telepresence, bridging geographic gaps, especially in rural or resource-limited settings. Digital models and simulations assist practitioners in preoperative planning, reducing intraoperative errors and improving outcomes. For instance, a case where XR aided in the successful separation of conjoined twins illustrates the potential for collaborative, global surgical planning using immersive tech.
Diagnostic processes are also transformed by AR/VR. Enhanced imaging techniques, such as AR overlays of MRI or CT scans directly onto patients, enable clinicians to identify issues more precisely. Digital twins further enable individualized care by modeling a patient’s unique anatomy and physiological parameters, supporting real-time monitoring and tailored interventions. To explore how AI supports medical decision-making, review how AI aids in delivering better healthcare.
Patients and Their Care
Patients benefit from AR/VR through improved engagement, education, and treatment adherence. Wearable sensors and head-mounted displays facilitate at-home health tracking for chronic conditions like diabetes, hypertension, and sleep disorders. Immersive therapies—such as VR relaxation environments—have demonstrated significant pain reduction during procedures like burn wound care, often decreasing perceived pain levels from severe to mild. For example, VR distraction techniques have shown promise in managing chronic pain conditions like fibromyalgia and phantom limb pain, with some studies reporting over 50% pain reduction.
VR-based pain management tools, such as RelieVRx, are now FDA-approved for in-home use, providing nonpharmacologic options for opioid-sparing pain relief. These innovations are especially impactful for vulnerable groups, including children and the elderly. Kids, for instance, use VR distraction apps during painful procedures, reducing anxiety and discomfort, although long-term safety data is still being developed. Similarly, elderly populations utilize XR to combat loneliness and facilitate social connection, which are critical for mental health and overall well-being. An example is Mynd Immersive’s platform, which has successfully reduced feelings of isolation among seniors in long-term care settings.
Medical Education and Workforce Development
XR has revolutionized medical training by offering realistic, reproducible simulations that surpass traditional cadaver-based or mannequin practice. Students and residents can perform complex procedures, emergency responses, and team-based scenarios in virtual environments, improving both technical skills and emotional preparedness. Studies indicate that VR-trained clinicians recall procedures more effectively and perform tasks faster than those trained via conventional methods. Incorporating XR into ongoing professional development helps address workforce shortages, especially in rural areas, while reducing training costs and logistical barriers.
Fostering a well-trained, tech-savvy healthcare workforce requires expanding XR training modules supported by federal agencies. Programs that integrate immersive tech into medical curricula and continuing education will prepare practitioners for the evolving landscape of digital medicine.
Overcoming Barriers and Managing Risks
Despite the promising potential, widespread adoption faces several hurdles. Cost remains a significant obstacle, with high initial investments required for hardware and software, especially for smaller hospitals and clinics operating under tight budgets. Workforce burnout and staff shortages further complicate integration efforts, as overburdened personnel may lack the time or training to implement new technologies effectively.
Regulatory pathways pose additional challenges. The FDA’s current classification system for AR/VR devices is evolving, but many head-mounted displays lack clear medical device designations, complicating approval processes. The absence of standardized quality metrics for XR imaging and therapeutics further impedes industry growth. Streamlining regulatory pathways through programs like the Breakthrough Devices Initiative and establishing comprehensive standards for image quality and usability are critical steps.
Privacy and security also require attention. XR devices collect sensitive health data, including biometric and behavioral information, necessitating robust safeguards aligned with existing laws such as HIPAA. Risks of cybersickness, eye strain, and psychological effects from extended use should be mitigated through ongoing research and user safety protocols. For detailed regulatory considerations, see the FDA’s questions to consider.
Policy and Investment Priorities
To accelerate XR integration into healthcare, policymakers should:
- Support federal privacy laws that harmonize data protection standards and clarify the scope of protected health information in immersive environments.
- Foster public-private partnerships, such as NIH’s BRAIN Initiative, to fund research and develop standards that catalyze innovation.
- Expand XR training modules within federally supported health workforce programs to ensure clinicians are prepared for digital care.
- Simplify FDA approval pathways by incentivizing the use of expedited review programs like the Breakthrough Devices Program and the De Novo pathway.
- Advocate for inclusion of XR-based therapies in Medicare and Medicaid coverage, utilizing existing coding systems and pilot programs like the Transitional Coverage of Emerging Technologies.
- Develop rigorous standards for XR hardware and software, ensuring high-quality imaging and ergonomic design.
- Increase federal funding for research into the long-term impacts of XR on health outcomes, especially among vulnerable populations like children and seniors.
These efforts will help unlock the full potential of AR/VR to transform healthcare delivery, improve patient outcomes, and maintain American leadership in medical innovation. For a comprehensive overview of standards and best practices, see the International Virtual Reality and Healthcare Association.
Conclusion
XR technologies are poised to redefine healthcare by enabling safer surgeries, more effective diagnostics, personalized treatments, and enhanced medical training. Strategic policy support, regulatory clarity, and targeted investments are essential to realize these benefits at scale. As AR/VR continue to mature, their integration into the health system can help bridge disparities, empower patients, and foster a new era of innovative, patient-centered care—ensuring the United States remains at the forefront of medical progress.